Long case
Date: 09- Feb-2021
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient- centered online learning portfolio and your valuable inputs on the comment.
A 50 year old female came to OPD with chief complaints of shortness of breath and bipedal edema.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 3years back, then she complaints of headache to which she was diagnosed as hypertension. She is on medication since then.
8months back, patient complaints of shortness of breath which is aggravated during supine position and she complaints of pedal edema which is pitting in nature and decrease urine output to which she was admitted to KIMS. She was diagnosed as chronic kidney disease. She was on maintenance haemodialysis since then.
She was undergoing two sessions of dialysis in one week.
Since one month, patient complains of fever which is high grade intermittent which subsides on medication and cough which is copious and non blood tinged.
Yesterday, she complaints of vomiting which is projectile , 3 -4 episodes in a day after a session of dialysis.
There is no history of sudden loss of weight.
PAST HISTORY:
She is a known case of hypertension since 3years and chronic kidney disease since 8months.
She is not a known case of Diabetes, asthma , COPD and tuberculosis.
PERSONAL HISTORY
Diet -mixed
Appetite- normal
Bowel and bladder habits- constipation
Sleep - adequate
FAMILY HISTORY:
There is no history of similar complaints in the family.
TREATMENT HISTORY:
Patient is not allergic to any known drug.
GENERAL EXAMINATION
patient was conscious,coherent, cooperative and well oriented to time, place and person.
Pallor is seen.
No icterus
No cyanosis
No history of generalised lympadenopathy
Bipedal edema is seen.
Temperature: afebrile
Respiratory rate: 18cpm
Pulse rate: 70bpm
Blood pressure: 130/90mm Hg
GRBS: 290
Spo2 at room temperature:99%
SYSTEMIC EXAMINATION:
Cvs examination:
Inspection :
No precordial bulge
No scars sinuses and engorged veins
No visible pulsation
Palpation:
apical impulse : heard in fifth inter coastal space
Auscultation:
S1 and S2 heard
No murmurs.
CNS examination:
Higher mental functions-normal
Cranial nerves- intact
Sensory system- normal
Motor system- normal
Meningeal signs- absent
Cerebellar signs- absent
Respiratory system examination:
Inspection of upper respiratory system-
oral cavity- normal
Nose- normal
Pharynx- normal
Lower Respiratory Tract:
Inspection:
trachea: central
Symmetry of chest : symmetrical
Movement: B/L symmetrical expansion of chest respiration
No scars, engorged veins or sinuses.
Palpation:
All inspectory findings are confirmed by palpation.
Trachea: central - confirmed by three finger test.
Assessment of anterior and posterior chest expansion- B/L symmetrical expansion of chest.
No chest wall tenderness
Vocal fremitus- normall
Percussion :
done in sitting position
Resonant
Auscultation:
Vesicular breath sounds heard
Bilateral air entry present
No added sounds
*Abdominal examination:
Inspection:
Shape : elliptical
Quadrants of abdomen moving in accordance with respiration.
No scars sinuses or engorged veins
Palpation:
No tenderness
No organomegaly
Percussion:
tympanicAuscultation:Normal
PROVISIONAL DIAGNOSIS:
CHRONIC KIDNEY DISEASE
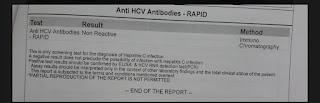
INVESTIGATION:
FINAL DIAGNOSIS:
CHRONIC KIDNEY DISEASE WITH MHD.
TREATMENT:
9th January
Tab NODOSIS 500mg BD
Tab NICARDIA 10mg BD
Tab LASIX 40mg BD
Tab ARCAMINE 0.1mg TID
Tab SHELCAL 500mg BD
Tab OROFERXT OD
Tab PAN 40mg OD
Inj Erythropoietin 4000 IV/SC weekly once
Inj IRON SUCROSE 1AMP in 100ml NS during dialysis
FLUID RESTRICTION<1l per day
SALT RESTRICTION<2.4g/day
10th january
Blood transfusion is done
Tab NODOSIS 500mg BD
Tab NICARDIA 10mg BD
Tab LASIX 40mg BD
Tab ARCAMINE 0.1mg TID
Tab SHELCAL 500mg BD
Tab OROFERXT OD
Tab PAN 40mg OD
Inj Erythropoietin 4000 IV/SC weekly once
Inj IRON SUCROSE 1AMP in 100ml NS during dialysis
FLUID RESTRICTION<1l per day
SALT RESTRICTION<2.4g/day



























Comments
Post a Comment